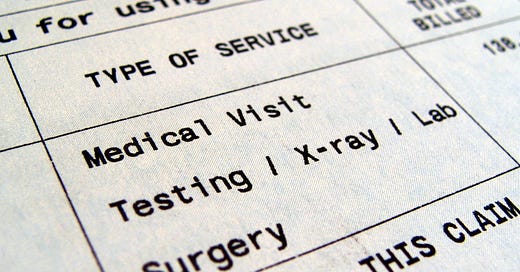
Cite HIPAA to Obtain Your Itemized Medical Bill and Billing Codes.
The federal privacy law requires medical providers and insurers to give patients their billing records. I've provided a helpful written template in this newsletter.
My friend Kay texted me the other day with an aggravating problem. She was getting the medical billing runaround.
What’s the medical billing runaround? It’s the vortex that entraps patients when their medical providers and insurance companies are passing the buck instead of correcting billing mistakes. You know you’re getting the medical billing runaroun…
Keep reading with a 7-day free trial
Subscribe to Marshall Allen Project to keep reading this post and get 7 days of free access to the full post archives.