Pause Before You Pay
Sam Radcliff took his wife to Mount Sinai’s emergency room in New York. The family received several bills afterwards, two of which were conflicting in nature.
Sam frantically took his wife to the ER while they were on vacation in New York. She had severe dizziness, vertigo, nausea, and vomiting — “the room was spinning like you’re on the Scrambler out of control at the amusement park.”
Sam Radcliff lives in North Carolina with his wife and four children. If Sam sounds familiar, it’s because he’s the same person featured in the last story about his colonoscopy and billing dispute with Novant Health. This time we’re unpacking an encounter he and his wife had with another health care system — Mount Sinai.
They were visiting New York City and were on Long Island when her vertigo symptoms began abruptly. Terrified and unsure of what was happening — and with disabling nausea — they sought emergency care at Mount Sinai South Nassau hospital in Oceanside on December 27, 2023.
“The symptoms were sudden and persistent at first. She had multiple episodes at the ER and was in agony and vomiting,” Sam said.
The ER was standing-room-only after the holidays amid flu, COVID, and RSV surges. Crowded winter ERs prioritize ruling out dangerous causes first. That often means imaging and labs before bedside maneuvers, especially when symptoms include vomiting, dizziness, and nausea. Based on her symptoms, medical journals document up to 15 different possible conditions. This makes determining an accurate diagnosis and a successful treatment plan challenging.
At the hospital Sam’s then 53-year-old wife saw half a dozen clinical staff, but no one landed on the specific type of vertigo during the five-and-a-half-hour visit. Based on her symptoms, the team prioritized ruling out dangerous conditions first.
“She saw about six or seven people over five-and-a-half hours… she was in agony,” Sam recalled. Claims show charges for labs, radiology (a brain CT, chest X-ray, and an EKG), medication, the ER, a medical group, and a physician group. The tests were important to rule out serious diagnoses including a heart attack, aneurysm or stroke.
They performed a brain CT without contrast and a chest X-ray — both with radiation exposure. The reasoning listed for the CT scan noted: “The room is spinning.” The chest X-ray reasoning stated: “dizziness.” They ultimately discharged her with a diagnosis of “general vertigo” and meclizine 25 mg.
Medical billing expert Dr. Shelley Safian weighed in with additional perspective: “These signs and symptoms are nondescript and point to more than one diagnosis. That makes determining an accurate diagnosis and treatment plan challenging. The labs were standard protocol to look for food poisoning, a stomach virus, dehydration, or metabolic imbalance. The same symptoms support a diagnosis of multiple sclerosis, migraine as well as labyrinthitis — hence the brain CT. Chest X-ray, EKG, and troponin look for a heart problem. Administering fluids and anti-nausea meds is standard to treat and prevent dehydration. The fact that tests were negative is part of the diagnostic process.” She added a broader point: “Most people believe there’s a straight line from signs and symptoms to diagnosis. There isn’t. Many conditions can present with dizziness, nausea, and vomiting. Careful rule-outs protect patients from catastrophic misses.”
Staff focused on her low blood pressure and discussed keeping her longer. “My wife was in no condition to make decisions, and I was out at the main desk,” Sam shared. Their 18-year-old daughter explained her mom’s blood pressure runs low, and she hadn’t eaten in 18 hours. After food and fluids, her blood pressure improved.
“They told her to go see her doctor. She was discharged without much having changed at all,” Sam said.
There are two main types of vertigo: peripheral and central. Peripheral vertigo is the most common and is caused by issues in the inner ear, while central vertigo results from problems in the brain, such as a stroke or tumor. Sam’s wife ended up having peripheral vertigo; the family inferred this shortly after leaving the ER following a basic online search of her symptoms. After returning home, they learned about the Epley maneuver — a simple positional technique that moves displaced ear-canal crystals back where they belong. Sam and his son helped Sam’s wife perform the maneuver several times and her vertigo cleared within 10 minutes. The successful Epley maneuver treatment confirmed a more detailed diagnosis which ended up being Benign Paroxysmal Positional Vertigo (BPPV) - a form of peripheral vertigo.
“We could have been out of the ER in 20 minutes if someone had said let’s try the Epley maneuver,” Sam said. “Google returned the result after we shared just a few symptoms.” From the family’s internet search and successful home remedy, they believe that Benign Paroxysmal Positional Vertigo (BPPV) is common and often straightforward to diagnose.
However, not all peripheral vertigo is BPPV, and canalith maneuvers like the Epley maneuver aren’t appropriate in every case.
Here’s the one-day claim summary across five claims:
Total Billed: $15,768.12
Plan Adjustments: $12,753.10
Allowed: $3,015.02
Plan Paid: $824.65
Patient Responsibility: $2,190.37
Total paid by Sam’s wife: $1,699.08
She’s covered by the North Carolina State Health Plan, administered by Blue Cross Blue Shield at the time. The state paid $824.65, and the family paid nearly $1,700 for the visit.
The effort and expertise were evident in the ER that day, but the family left frustrated as the vertigo symptoms were still present at discharge. It took Sam and his family being resourceful to find an effective remedy themselves.
Service highlights by entity (billed; allowed) are below.
Mount Sinai South Nassau Hospital (professional radiology):
Chest X-ray interpretation ($32.00; $14.27)
Brain CT interpretation ($143.00; $64.90)
Mount Sinai Marathon Medical Group:
EKG interpretation ($50.00; $15.89)
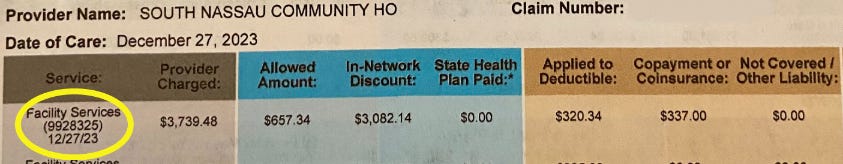
South Nassau Community Hospital (facility, tests, meds):
ED visit, moderate complexity ($3,739.48; $657.34)
IV push ($2,247.42; $395.06)
Labs: CMP, CBC, troponin, CK (various)
Chest X-ray ($768.51; $135.09)
Brain CT ($4,984.88; $876.26)
Pharmacy, fluids, meds (various)
EKG technical component ($654.49; $115.05)
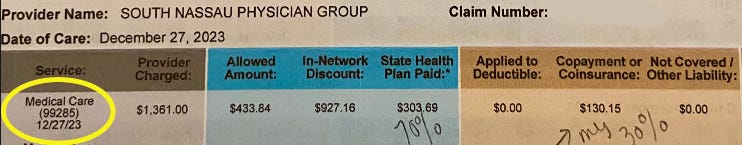
South Nassau Physician Group:
ED E&M, highest level ($1,361.00; $433.84)
Night services ($50.00; $0.00)
Sam’s wife went to one hospital, but she received bills from four different groups - a dizzying reality of modern medical billing.
What jumped out: the physician group billed a level 5 Evaluation and Management (E&M) while the hospital billed a level 3 E&M. Two entities, same patient, same encounter — incongruent E&M levels. Based on the general vertigo diagnosis, that looks like potential upcoding or at least inconsistent documentation between teams.
Screenshots of the two claims show the incongruency.
Screenshots of mailed claim statements the family received from BlueCross BlueShield of North Carolina.
On vertigo treatment and coding, Dr. Safian noted: “The Epley is part of a procedural code which groups canalith repositioning procedures ‘per day.’ It’s not billed as a standalone unique code and is often considered part of managing the condition under E&M. The ED may not attempt it unless BPPV is reasonably confirmed. In a very busy ED, triage and competing priorities can push a stable vertigo case to discharge with follow-up.”
Agency for patients in real time: in the ER, ask what each test is ruling out, whether a bedside positional test is appropriate now, and if any test can safely wait. If discharged without relief, ask for specific follow-up instructions and what warning signs require immediate return.
“They [South Nassau Hospital ER] were not as thorough as they could have been in a perfect world, and the family has every right to feel upset. But vague symptoms can point to many serious diagnoses. Careful rule-outs protect patients — and sometimes the win is confirming what it isn’t,” Dr. Safian shared.
Across five claims, the family received more than a dozen bills. Two went to collections while they tried to negotiate — and ended up with two different collectors despite one encounter.
After insurance adjudication, they saved nearly $500 by waiting to reach a representative willing and authorized to negotiate. “Our portion wasn’t a large percentage, but we were so frustrated they missed a simple diagnosis and remedy,” Sam said. He was told many times that charges aren’t negotiable. He persisted.
In September 2025, almost two years after the visit, one $1,965.16 bill (then in collections) got an initial $350 reduction. After he paused, the offer improved; he paid $1,473.87 within 48 hours.
After reading Never Pay the First Bill, Sam often sees 30% discounts by waiting a few cycles on prices that aren’t fair. He checks Fair Health Consumer and uses online tools to gauge reasonable charges. Those data points fuel his confidence and negotiation strategy.
“I wind up having to negotiate everything because I so rarely get a full and honest answer,” he said.
There’s no win that is too big or too small. If you or anyone you know has a Victory Story to share, please reach out.
Key Takeaways:
1. One Medical Visit Can Generate Multiple Bills
Even a single emergency room visit can result in separate bills from multiple providers, often arriving weeks or months apart. Patients should never assume the first bill is the final bill.
Why this matters:
People often pay early bills out of fear, only to discover later charges they didn’t expect or understand.
2. Insurance Coverage Does Not Guarantee Fair Pricing
Being “covered” does not mean:
All providers are in-network
Charges are correct
Prices are reasonable
Why this matters:
Patients need to review every charge, even when insurance is involved.
3. Errors Are Common—and Often Correctable
Coding mistakes, duplicate charges, and misapplied rates appear frequently in medical bills. In this case, persistence and documentation made a real difference.
Why this matters:
Billing errors are not rare exceptions. They are a predictable part of the system.
4. The Fight Often Happens After the Care
The most difficult part of healthcare isn’t the treatment—it’s the administrative aftermath. The system counts on patients being tired, intimidated, or unsure of what to ask.
Why this matters:
Knowing when to engage (after the visit) is just as important as knowing how.
5. Persistence Changes Outcomes
This story reinforces a central Marshall Allen principle:
Polite persistence works.
Asking for itemized bills, following up, escalating when necessary, and documenting conversations can materially change what a patient ultimately pays.
6. You Don’t Need to Be an Expert—You Need a Process
The people who succeed aren’t billing professionals. They’re patients who:
Ask questions
Request documentation
Take notes
Don’t accept the first answer
Why this matters:
This is exactly where tools like the MAC—and trained advocates—add value. Sam saved nearly $500 by waiting out collections and pushing for a fair deal. Never pay the first bill. Dispute debts in writing—use the Marshall Allen Clone to help with a template. Read Never Pay the First Bill for the full playbook.